Blog

August 22, 2025
Position your ACO for success with a focus on the basics
Lindsey McCreary
Lindsey is a senior director in provider sales at Vatica Health.
Headwinds facing health systems these days include declining reimbursements, staff shortages and patients seeking care outside the system. For organizations with Medicare ACOs, the Centers for Medicare and Medicaid Services (CMS) has proposed an accelerated timeline to take on downside risk for Original Medicare patients. Because of this change, health systems not already earning ACO shared savings may face additional revenue challenges due to shared loss exposure in more advanced ACO models.
Successful health systems will get ahead of these trends by mastering the basics. One of the most crucial is accurate documentation by providers participating in ACO REACH (Accountable Care Organization Realizing Equity, Access, and Community Health) and MSSP (Medicare Shared Savings Program). Here’s why:
- Accurate risk adjustment and reimbursement. Accurate coding ensures that providers are appropriately compensated for the complexity of their patient population. Diagnosis codes must be backed by clear, specific and complete documentation. Without this, codes may be rejected during audits, leading to lower risk scores and reduced reimbursement
- Quality performance measurement. Both MSSP and ACO REACH reward high-quality, cost-efficient care. Quality scores influence shared savings distribution, while coding and documentation directly impact quality metric performance (e.g., preventive screenings), which are derived from reported data.
- Compliance and risk mitigation. Like health plans, providers must prepare for RADV audits. Inadequate documentation can lead to repayment demands and compliance issues. Thorough documentation serves as a legal record, mitigating potential liability.
- Improved patient care and care coordination. Comprehensive documentation improves care team visibility into a patient’s health status, enabling better coordinated, timely and personalized interventions. This is critical in value-based models where proactive management of chronic and complex conditions is a key success factor.
- Strategic decision-making and population health. Coding data powers analytics used to stratify risk, track population health trends and allocate resources efficiently. ACOs should use this information to design targeted care programs, such as intensive case management for high-risk patients. Coding accuracy also influences benchmark setting in MSSP and capitation payment calculations in ACO REACH, affecting financial viability and strategic planning.
Challenges to accurate coding and documentation for an ACO include variation among employed and community providers, as well as multiple platforms on multiple EMRs. Given ongoing margin pressures, many health systems lack the resources to build and sustain a robust internal coding program.
Success factors
Without accurate documentation, ACOs don’t receive the revenue necessary to care for their patients. Inadequate benchmarking also affects an ACO’s ability to tackle social determinants of health (SDOH), which can significantly impact a patient’s overall health status.
Ensuring a productive Annual Wellness Visit for Medicare patients helps ACOs to identify, code and document risk-adjustable conditions. This visit is also an opportunity to identify and close care gaps. Leaning into quality programs unlocks the potential to keep patients healthy and receive additional revenue.
The focus on chronic conditions and care gaps has another benefit: it enables the generation of additional downstream revenue from screenings, lab work and specialty referrals. Data shows that on average, approximately $6,000 per Medicare patient per year can be generated annually by providing necessary and appropriate care.*
An ACO should ask the tough questions about what’s hindering the organization. Is the program too cumbersome or complicated for physicians to use? Are physicians not engaged? Would they benefit from education about the importance of this work?
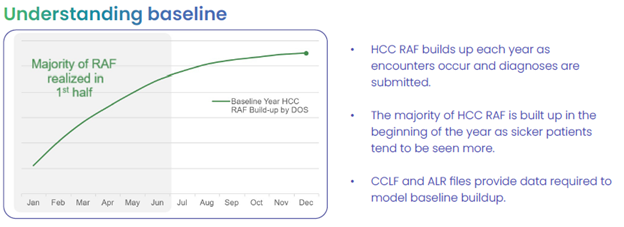
RAF accuracy progression
For many ACOs, outside expertise can reduce total cost, driving further financial opportunity. For example, Vatica Health employs dedicated nurses to synthesize EMR and ACO data, reducing noise presented to providers. This concise, accurate information helps the provider make the most of the visit to address risk-adjustable conditions and care gaps.
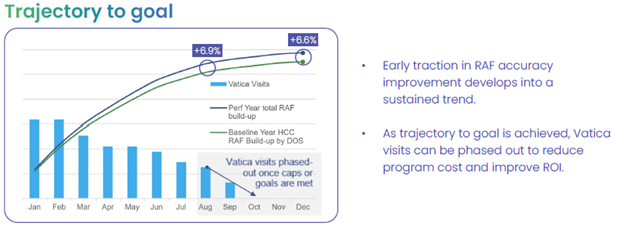
Vatica helps ACOs understand the patient population and focus on patients the data suggests may have undocumented conditions. The Vatica team can help ACOs reach patients earlier in the performance year to impact their health outcomes quickly and build HCC RAF.
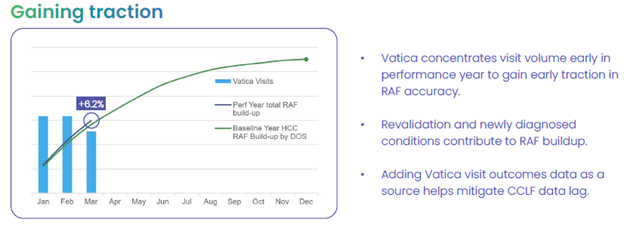
Vatica’s solution accounts for annual risk adjustment parameters of the MSSP and REACH program so ACOs can adjust as they get closer to goal. And Vatica is paid based on the number of completed visits only. Any shared savings stays with the organization to reinvest in patient care and compensate providers.
In ACO REACH and MSSP, coding and documentation are foundational to financial sustainability, compliance, quality performance and excellent care. Organizations that invest in robust documentation practices and risk-adjustment coding accuracy are better positioned to thrive in value-based care environments. They can then focus on cost management, delivering better care and more effective oversight of the full patient journey.
*McKinsey and Company citing based on data from Vatica Health, Centers for Medicare and Medicaid Services, Physicians Practice, American Medical Association, Cancer.org, National Library of Medicine and American Journal of Preventive Medicine.
Report
Value-based care survey
Physicians and executives give practical feedback from the front lines. To assist in your transition to VBC, learn new findings from your colleagues who are experiencing its various challenges and opportunities.
Learn more »
Resources
Read our latest thoughts
on healthcare

Subscribe to Vatica Voice
Get our latest news and insights delivered directly to you.
Adjust your approach to risk adjustment
Talk to one of our risk adjustment experts today to see how we can help you deliver better performance and stronger compliance while closing gaps in care.