
By Brian Flower, vice president of client solutions, Vatica Health
Health Affairs recently published a study of data from 4 million Medicare Advantage (MA) members indicating that health risk assessments (HRAs) contributed up to $12 billion per year to risk adjusted payments in 2020. This is based on conditions that were submitted exclusively by an HRA (not submitted through another encounter) during the 2019 calendar year. The study implies that HRAs, typically performed in-home by vendors on behalf of MA plans, can lead to inflated hierarchical condition category (HCC) scores. More specifically, of the 44.4% of MA beneficiaries who had an HRA, HCC scores increased on average 12.8%.
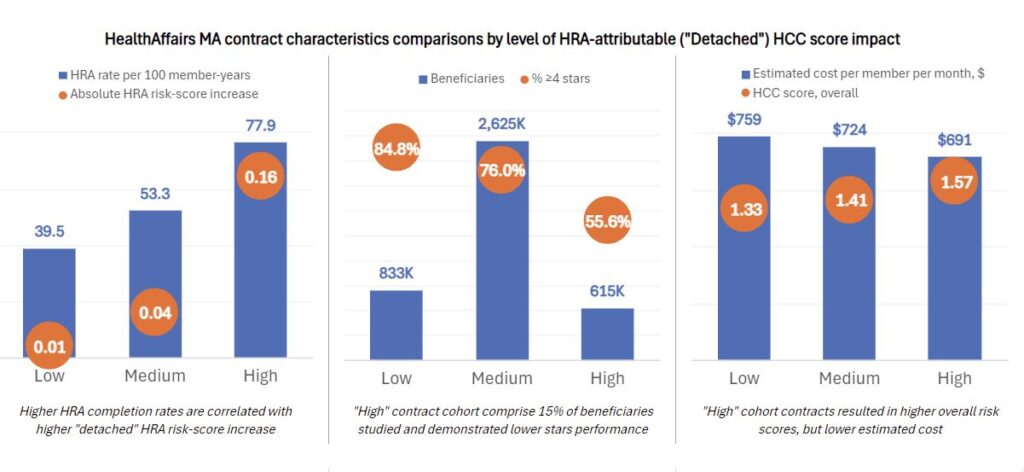
Study authors go a step further by segmenting contracts as low, medium and high, based on the HRA’s effect on risk score at the contract level. This may provide insights into HRA program design by the plan, e.g., which patients are targeted and how HRA outcomes are subsequently attached to care management.
For nearly a decade, the Centers for Medicare and Medicaid Services (CMS) and the Office of the Inspector General (OIG) have expressed concern with the improper use of HRAs to inflate payments, rather than to improve care and outcomes. While HRAs can be a helpful tool for plans to identify all active conditions on an annual basis, the disconnect or “detachment” arises when diagnoses captured in HRAs are not recorded in a subsequent medical visit. This undermines the purpose of risk adjustment, which is designed to compensate plans based on the expected costs of delivering benefits to enrollees.
Key observations
- The population was designated as follows: 20% low, 15% high and the remaining 64% in the medium cohort.
- While comprising only 15% of enrollees, the high cohort accounts for 48% of the total HRA risk-score increase.
- The HRA rate was much higher in the high contracts (77.9%) than low contracts (39.5%).
- Quality ratings favored low cohort contracts with 85% 4 stars or better vs high cohort contracts at 56%.
- Provider and health system integration was dramatically higher in the low vs the high contract cohort.
- Comparing the high and low contract cohorts, while the overall HCC score was 18% higher, medical expense was 9% lower (estimating from the plan payment and medical loss ratio values provided).
Extrapolating on the points above, PCP-integrated risk adjustment solutions drastically reduce the risk of detached HRA outcomes and quality performance. This stands to reason because the patient’s PCP is prioritizing healthcare outcomes and management of chronic conditions, rather than focusing exclusively on code capture.
The correlation between HRAs and coding intensity is particularly relevant given the Risk Adjustment Data Validation (RADV) Final Rule, which authorizes CMS to extrapolate RADV audit findings beginning with payment year 2018, applying the error rate from a sample, and the associated financial penalties, across a broader population of the Medicare Advantage Organization’s contract. In a RADV audit, conditions supported by a single encounter, like detached HRA visits, are at higher risk because there are no additional medical records to fall back on if there is an access, accuracy, or completeness issue with the primary record. A PCP-integrated approach encourages follow-up care and additional documentation to support valid diagnoses.
It should be noted that this study uses the 2020 CMS risk adjustment model. We expect the exclusive impact of HRAs on risk scores would be tempered by as much as 40% using the 2024 risk adjustment model, which is being phased in now and will take full effect for 2025 dates of service.
Conclusion
At-risk entities should evaluate their current risk adjustment programs and focus on solutions that produce accurate and compliant coding accuracy that dovetail with quality and health outcomes. Legacy programs, such as retrospective chart reviews and HRAs completed by in-home assessment vendors, should be augmented with a provider-centric approach. Build a risk adjustment strategy that recognizes PCPs as partners in accuracy and quality capture, as well. PCPs are best positioned to capture all existing conditions and to address the CMS and OIG’s concerns by connecting the dots between accurate HCC capture and improved care and outcomes.








Recent Comments