
2021 has been a challenging year for primary care physicians nationwide. They’ve risen to the challenge by remaining committed to providing value-based patient care during times of intense operational transformation and financial uncertainty. However, it hasn’t been without sacrifice. Sixty-six percent of primary care physicians say they often experience feelings of burnout. This isn’t surprising given the risks associated with COVID-19 exposure as well as the significant burden of non-clinical work that requires their time and attention. Internists, for example, spend nearly 20 hours per week on paperwork and administrative tasks. Nearly a quarter of physicians (23%) say the most challenging part of their job is navigating ever-changing managed care and regulatory compliance requirements. The silver lining is that COVID-19 cases are declining and there are solutions to help you improve clinical and financial performance.
With only a couple of months remaining in 2021, there are several steps you can take to ensure that your practice meets all performance targets and that your patients receive the highest quality of care. The good news is that most of these actions are often supported by payer-sponsored risk adjustment and quality programs that provide vital clinical and administrative support to practices. This support helps providers close care gaps, enhance coding and documentation, identify and assess social determinants, and perform patient outreach. To enhance performance under value-based care contracts, consider these 10 tips:
1. Review 2021 performance reports from payers. These reports are a treasure trove of information and identify opportunities for improvement. Common examples include patients without primary care office visits, patients for whom chronic conditions were coded in 2020 but not recaptured in 2021, patients with incomplete preventive screenings, and patients with open gaps in care. Gather internal resources and put action plans in place.
Keep in mind that data latency may result in delayed reporting. Consequently, best practice is to compare external reports with your patients’ medical records for confirmation. Your practice’s EMR may include information that has not yet been reported to managed care plans. This information may impact your performance in value-based care programs. Perform a thorough reconciliation of all data sources to ensure consistency, alignment, and accurate performance reporting for all patients.
2. Ensure all eligible patients have completed an annual preventive care office visit. Schedule annual wellness visits (AWV) and other preventive care visit types for eligible patients. These visits provide opportunities for each patient to complete their personal prevention plan and Health Risk Assessment. Annual physical exams allow physicians to address care gaps as well as proactively identify potential chronic conditions. Check patients’ records when they present for a sick visit and schedule applicable preventive visits. For patients who have not visited the office, proactive patient outreach signals that you care about their well-being and that your office is there to help. Remind them they’re due for a visit and assist with scheduling. These actions foster trust and build stronger patient-physician relationships.
3. Follow up with patients who miss scheduled appointments. Consider whether any of your patients are missing appointments or not accessing routine care due to socioeconomic barriers?
Social determinants have a significant impact on health outcomes. As such, it is important to proactively reach out to vulnerable patients and address those barriers? The American Academy of Family Physicians provides some helpful advice.
4. Follow up with patients who were referred for preventive screening but did not comply. Patients’ needs and challenges vary. While some may have forgotten about the recommended screening, others may be experiencing difficulty scheduling the appointment due to long call wait times or limited appointment availability. Others may have unanswered questions that prevent them from taking action. The best practice is to call patients directly, assess the barrier, and determine what the practice can do to help. Oftentimes, a reminder call is all that’s needed.
5. ‘Close the loop’ with specialists. Communication between primary care physicians and specialists is important to avoid fragmented care delivery and ensure patient satisfaction. Ensure care continuity by following up with any specialists to whom patients are referred. Request findings and recommended treatment plans, as applicable, an update your EMR with relevant clinical information.
6. Keep close tabs on patients with multiple chronic conditions or who are on multiple medications. Do patients take medications as prescribed? Are their chronic conditions controlled, or are they at risk of acute exacerbations? The goal is to keep patients healthy and out of the hospital. If your practice hasn’t yet started a chronic care management program, now is the time to do it. For elderly patients who are on high-risk medication regimens, conduct a thorough evaluation, and consider lower-risk alternatives.
7. Conduct patient outreach after an acute event or hospitalization. Schedule appointments to review aftercare plans and make sure patients understand and can implement these plans. Do patients understand the specialists with whom they must follow up? Do they know what medications they must take? Do they know who to contact if they have questions? Can they recognize signs and symptoms that would warrant a phone call to their doctor? These are important questions to review with your patients.
8. Evaluate office workflows. Focus on preventive care, prioritization of high-risk patients, coordination of care, and strong communication with other members of each patient’s care team. Where are the deficiencies and how can the team improve processes? Research and evaluate technology solutions that can seamlessly integrate with your office’s existing systems and improve workflows while reducing operating costs.
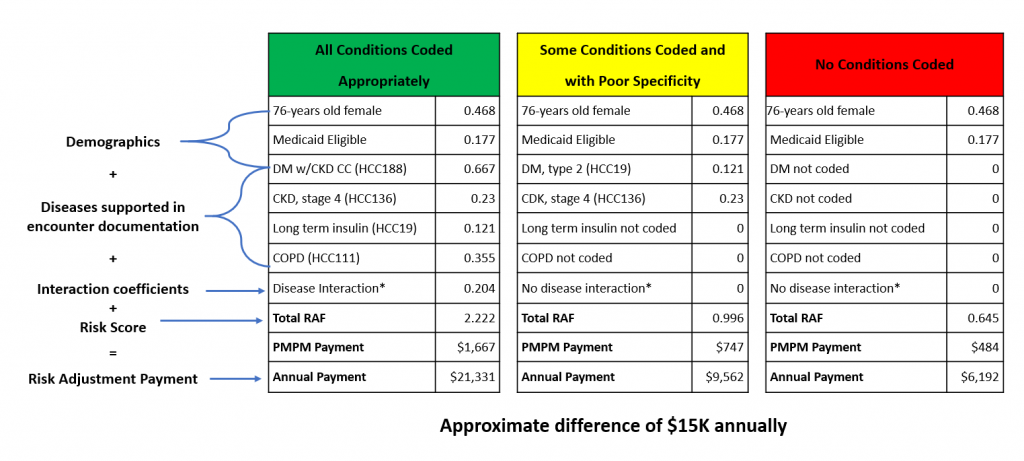
9. Improve documentation and coding accuracy. Schedule dedicated time for role-specific training and education that includes front office staff, medical coders, and providers. Individuals serving in each of these roles must understand how their actions (or inactions) impact the accuracy and specificity of medical record documentation and coding. This information directly impacts performance calculations, care delivery, and potential payments.
10. Leverage free external resources. External resources such as local community programs can often provide support for patients and serve as an extension of your practice through their focus on improving quality of life. For example, there are programs that can help address social determinants of health. Additionally, health plans sponsor risk adjustment and quality programs that provide clinical and administrative resources to support primary care practices. Leveraging these programs improves quality of care and patient satisfaction while reducing the burden on physicians. This, in turn, reduces the risk of burnout and attrition.
How Vatica Health can help
Founded in 2011 as the first preventive services technology solution designed specifically for physicians, by physicians, Vatica Health remains a pioneer in physician-centric technology and support solutions that directly improve clinical outcomes, efficiency, and financial performance. Vatica Health deploys on-site or virtual licensed, clinical nurses that serve as extensions of your team at no cost to the practice. Vatica Health is accelerating the transformation to value-based care by helping providers, health plans, and patients work together to achieve better outcomes. To learn more, visit https://vaticahealth.com/.




Recent Comments