
Q&A with Vatica Health Co-Founder, Dr. Averel Snyder
At Vatica, we pride ourselves on being a company founded by physicians for physicians. Dr. Averel Snyder, a cardiothoracic surgeon, cofounded Vatica in 2011 after becoming frustrated with the mounting challenges physicians were facing. He set out to create a unique PCP-centric model that places providers in the driver’s seat of improving both quality of care documentation and practice revenue. We recently spoke with Dr. Snyder to discuss why he started Vatica and how risk adjustment and quality initiatives fit into broader, and timelier, industry issues including value-based care, the role of the PCP, and the COVID-19 pandemic.
There are not a lot of companies that solely focus on enabling physicians to perform risk adjustment coding and quality of care initiatives. What inspired that for Vatica?
It’s a funny story. Steve, my co-founder, and I initially started Vatica nearly a decade ago to enable physicians to more efficiently deliver the newly created Medicare Annual Wellness Visit. We knew that once we helped providers improve care and practice revenue, we could offer more comprehensive solutions. A couple of years later, I was attending a healthcare conference, listening to the CEO of a home assessment company boast about the benefits of his organization versus alternative methods of capturing diagnostic codes for the purpose of risk adjustment. He stated emphatically that their model was the best method for optimizing risk adjustment coding and stratifying patient risk, which enabled their health plan clients to accurately predict the costs on which their capitated payments are based. As he spoke, I felt myself becoming more frustrated by the minute because his claims seemed unfounded.
Immediately, I thought, this isn’t fair or accurate for a few reasons. First, PCPs are inappropriately being cut out of the financial and care loop. Second, it’s not in the patients’ best interest to be seen by a clinician with whom they have no relationship with and who does not have access to their complete medical record. Third, I wondered how non-PCP affiliated nurses were closing clinical and quality care gaps.
I went home and began to research the Medicare Advantage industry and quickly found that my concerns were justified—CMS also began to scrutinize the value of home assessments that failed to improve care and outcomes due to the lack of integration with the PCP.
I had the proverbial light bulb moment. It struck me that we should empower physicians to use a simple interface to perform risk adjustment coding and capture quality of care data in a way that also improves their practice’s financial performance. I knew this could address an important pain point that most physicians feel—being overworked and underpaid. Plus, I knew that the treating physicians could do this work with greater efficiency and quality, leading to improved patient outcomes.
Fortunately, this insight, unlike many of my other entrepreneurial ideas, proved accurate, and nearly a decade later we have empowered thousands of PCPs to “take back” risk adjustment assessments. In doing so, we’ve helped improve outcomes and generated tens of millions of dollars for our provider network.
What makes Vatica’s solution different?
As a busy practicing physician for over two decades, I think I have a good sense of what frustrates providers—too many administrative burdens, not enough time, and declining income. We designed our solution with these frustrations in mind. We provide dedicated clinical support services to reduce administrative burdens, we negotiate health plan incentives to enhance PCP revenue, and improve quality by increasing the use of preventive services and helping to close care gaps. It’s a win-win-win—providers, health plans, and patients all benefit.
Why is it important to put PCPs at the center of risk adjustment?
I feel strongly that the PCP should be at the center of care. The treating PCP and their staff—not some randomly assigned clinician—is best suited to have the most efficient and effective face-to-face encounter with the patient. Given their relationship with the patient and access to all clinical information in their EMR, they are the most appropriate clinician to accurately document and code clinical conditions and close care gaps leading to better outcomes.
Talk to us about how Vatica helps PCPs succeed in value-based care.
Value-based care is about efficiently providing the highest quality of care to improve outcomes. There are a number of studies that demonstrate physicians in value-based care programs provide higher quality of care. Unfortunately, many PCPs lack the technology, expertise, staff, time, and other resources to thrive in value-based care. Vatica addresses this issue head-on. Unlike a lot of other solutions, Vatica is not here to make more work—we actually do 90% of the work for PCPs.
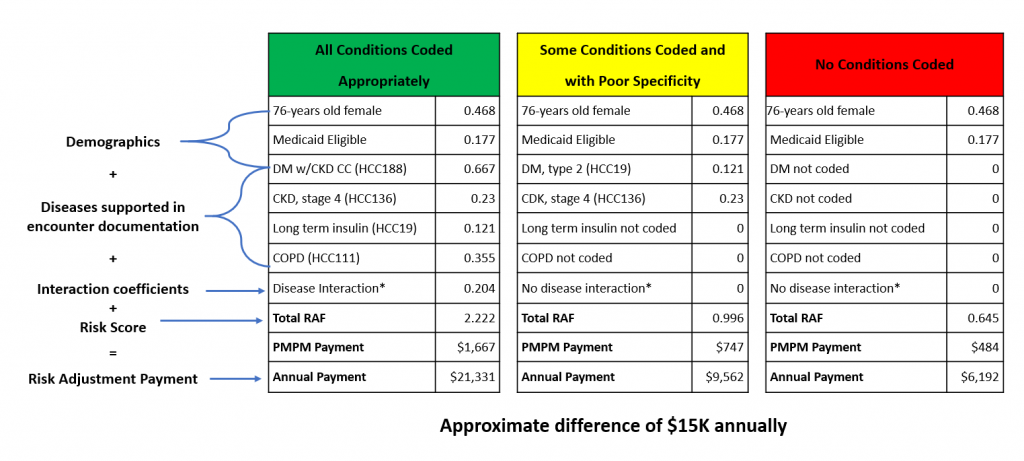
Vatica’s solution not only facilitates risk adjustment documentation and coding—but also enables PCPs to close gaps in care and increase the utilization of preventive services which are critical to improving outcomes. Powered by our technology platform, PCPs accurately capture all the active medical conditions with the associated documentation for clinical validation in the medical record. Vatica’s clinical consultants leverage all available data to create an accurate and complete view of the patient—the key to improving outcomes and performance in value-based care.
Why are risk adjustment and quality of care initiatives important to primary care providers?
Value-based care is designed to incentivize providers to improve outcomes in a cost-efficient manner. Finances and quality of care are inextricably linked. Success in value-based care depends on accurately assessing the needs of your population so that your payments will be sufficient to deliver appropriate care. And for PCPs, this should be an urgent initiative since each year alternative payment models shift more risk to providers. I’ve heard providers say, “When value-based care comes, then I will pay attention to risk adjustment.” But, then it’s too late. The CMS data collection lags approximately three years, so your allocated resources for patient care in 2021 may be dependent on your coding and documentation in 2018. The time to focus on it is now.
What are the compliance risks for PCPs and health plans with other risk adjustment and quality of care solutions?
In a standard risk adjustment data validation audit for a health plan, a meaningful percentage of the submitted diagnosis codes will be unsubstantiated in the medical record. Most of the approaches to risk adjustment are not meeting the new standard, which requires clinical validation. As a physician, it was important for me to design a solution that improved efficiency and mitigated compliance risk for providers. To accomplish this goal, we aggregate all available clinical data from the EMR and present all active medical conditions and their associated documentation for clinical validation to the treating provider. The provider is then responsible for selecting an appropriate ICD-10 code and completing “TAMPER” documentation. Then, as a fail-safe, after the provider e-signs the visit, we ensure that 100% of the codes are reviewed for completeness and accuracy by our team of AAPC CRC™ certified nurses, prior to submitting the codes to the health plan. We also deliver comprehensive provider ICD-10 coding and documentation training, which I personally provide and oversee.
What keeps you up at night in the current situation, with all the changes and disruptions in care during the pandemic?
PCP practices, particularly those who serve seniors, have endured some serious challenges. Reimbursement models are changing, and the new models demand vigilant documentation, accurate coding, additional practice resources, and subject matter expertise lacking by most physicians. At the same time, health plans are struggling to maximize risk adjusted revenue to ensure that seniors, who are the most vulnerable and costly patients, are receiving quality care and improved outcomes. Fortunately, CMS approved telehealth for a variety of encounters, including risk adjustment, and in-office patient volume has also started to bounce back from the post-pandemic decline. I think CMS will have to continue to adapt and make changes to the Medicare Advantage HCC model to account for the missed outpatient care during the pandemic. I am concerned about the increasing demands and worries of the PCPs, but I am optimistic about our ability to be a true partner, and subject matter expert, to help them succeed in this everchanging environment.
To learn more about how Vatica helps providers, watch our quick overview video.











Recent Comments